
Internal Medicine Residency at Maimonides Medical Center
Maimonides Internal Medicine Residency
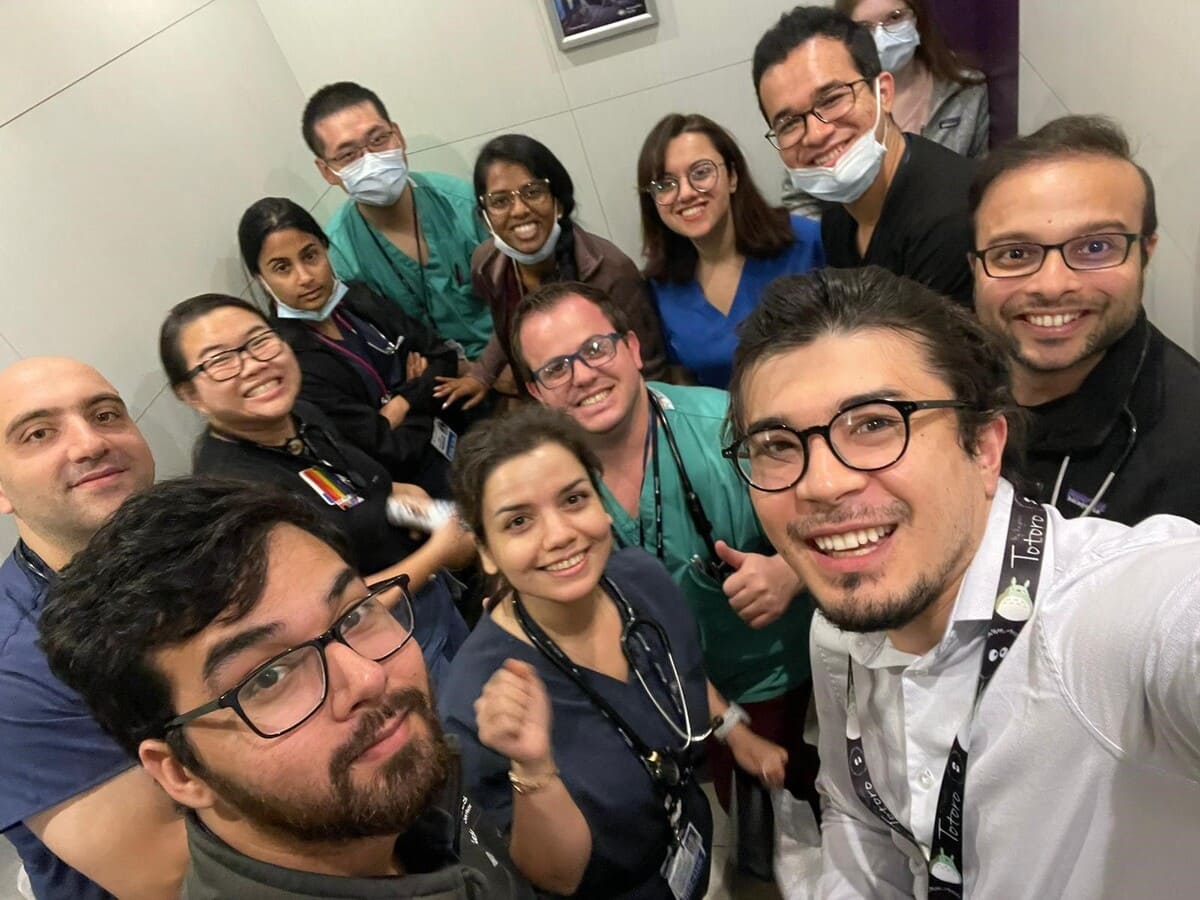
The residents of the Maimonides Medical Center Residency Program are what make our program special. Our trainees come from all over the world with varied experience and knowledge that they bring to our program.

















Care Visits
Discharges
Members
Subspecialty Fellowships
Chief Residents

Britney Chukwuka
Hometown: Silverdale, Washington
Medical School: St. George’s University
Interests: Medical Education, Clinical Teaching, Patient Advocacy
Fun Fact: Middle child of seven siblings. Welcomed her first child during chief residency. Studied fine arts in Italy, and is a licensed cosmetologist.

Tejaswi Venigalla
Hometown: Guntur, India
Medical School: Jiamusi Medical College
Interests: Clinical Research, POCUS, Medical Teaching and Hematology & Oncology
Fun Fact: Speaks Hindi, Telugu and Chinese. Loves to travel and making Biryani for family and friends.

Alana Zanetti Yabur
Hometown: Caracas, Venezuela
Medical School: Universidad Central de Venezuela
Interests: Medical Education, Hospital Operations, Gastroenterology and Advance Endoscopy
Fun Fact: Speaks Spanish and Italian. Has been practicing Yoga for 18 years. Loves hosting dinner for loved ones.

Shehanaz Shajahan
Hometown: Kerala, India
Medical School: K.S. Hedge Medical Academy
Interest: Clinical Teaching, POCUS, Critical Care and Infectious Diseases
Fun Fact: Was raised in Dubai. Loves baking and will hopefully open a pastry shop some day!
Graduates from our residency program go on to fellowships, primary care, and hospitalist positions around the country







Class of 2023
- Supraja Achuthanandan, Maimonides Medical Center, Brooklyn, NY
- Arjun Basnet, Reading Hospital – Tower Health, Reading, PA
- Amit Gulati, Mt. Sinai Beth Israel, Manhattan, NY
- Cece Ibeson, HonorHealth, Phoenix, AZ
- Ifeanyi Nwosu, Maimonides Medical Center, Brooklyn, NY
Class of 2022
- Sehajpreet Singh, Maimonides Medical Center, Brooklyn, NY
- Emanuel Emeasoba, Maimonides Medical Center, Brooklyn, NY
- Bruno De Brito Gomes, Maimonides Medical Center, Brooklyn, NY
- Chad Harris, University of South Florida, Tampa, FL
- Sanchit Kundal, Mount Sinai Beth Israel/Morningside, Manhattan, NY
- Alejandro Munoz-Martinez, Maimonides Medical Center, Brooklyn, NY
Class of 2021
- Nnamdi Chukwuka, Maimonides Medical Center, Brooklyn, NY
- Tomer Hananya, Maimonides Medical Center, Brooklyn, NY
- Mahsa Pourabdollah Tootkaboni, Maimonides Medical Center, Brooklyn, NY
- Aparna Tiwari, Maimonides Medical Center, Brooklyn, NY
- Ori Waksman, Medstar, Georgetown, DC
Class of 2020
- Nana Gegechkori, Maimonides Medical Center, Brooklyn, NY
- Dikshya Sharma, Westchester Medical Center, NY*
Class of 2019
- Paurush Ambesh, University of Massachusetts Baystate Medical Center, MA
- Arsalan Hashmi, Maimonides Medical Center, Brooklyn, NY
- Sarah Rosanel, Maimonides Medical Center, Brooklyn, NY
- Nitin Sabharwal, Tulane University, NO
- Vineet Meghrajani, Mount Sinai Beth Israel, NY
- Cynthia Balasanmugam, Maimonides Medical Center, Brooklyn, NY*
- Isaac Mizrahi, University of Hawaii*
Class of 2018
- Chaya Levine, Maimonides Medical Center, NY
- Isaac Akkad, NYU Winthrop Hospital, NY
- Parul Kakar, Rutgers University, NJ*
- Carlos Henriquez-Felipe, Maimonides Medical Center, NY*
- Kelsey Shanahan-Prendergast, Kelsey-Seybold Clinic, TX
Class of 2017
- Azizul Rehman, SUNY Downstate, NY
- Avraham Miller, Maimonides Medical Center, NY
- Shiv Raj, Maimonides Medical Center, NY
- Sabah Siddiqui, Maimonides Medical Center, NY
Class of 2022
- Suhali Kundu, George Washington University/MedStar Health, DC*
Class of 2021
- Kriti Gupta, Maimonides Medical Center, Brooklyn, NY
- Kiran Para, Maimonides Medical Center, Brooklyn, NY
Class of 2020
- Sanwal Mehta, Maimonides Medical Center, NY
Class of 2019
- Jevon Samaroo-Campbell, SUNY Downstate, NY* (Infectious Disease/Critical Care)
- Raphael Ezeagu, Maimonides Medical Center, Brooklyn, NY
Class of 2018
- Vignesh Ponnusamy, Maimonides Medical Center, NY
Class of 2017
- Olaoluwatomi Lamikanra, Maimonides Medical Center, Brooklyn, NY
Class of 2023:
- Tiffany Lu, Montefiore Medical Center, Bronx, NY
Class of 2021
- Mo Mai, SUNY Downstate, Brooklyn, NY
Class of 2020
- Suruchi Karnik, SUNY Downstate, Brooklyn, NY
Class of 2018
- Sujata Shrestha, SUNY Downstate, Brooklyn, NY
Class of 2017
- Deepa Vincent, University of Massachusetts, MA*
- Lina Soni, SUNY Downstate, NY
Class of 2023:
- Neha Sharma, Maimonides Medical Center, Brooklyn, NY
- Avleen Kaur (Hepatology) Montefiore Medical Center, Bronx, NY
Class of 2021
- Samantha Erlich, Maimonides Medical Center, Brooklyn, NY*
Class of 2020
- Kaveh Zivari, Maimonides Medical Center, Brooklyn, NY
- Steve Obanor, Maimonides Medical Center, Brooklyn, NY
- Fidelis Okoli, NYU Winthrop Medical Center, NY
Class of 2019
- Daria Yunina, Maimonides Medical Center, Brooklyn, NY
Class of 2018
- Zain Sobani, University of New Mexico, NM
- Alexa Sasson, University of Toronto, Canada
Class of 2017
- Richard Fazio, Maimonides Medical Center, Brooklyn, NY
- Bridget Gallagher, SUNY Downstate, NY
Class of 2020
- Aviva Tobin-Hess, Long Island, NY
- Vivian Zhu, Maimonides Medical Center, NY
- Goel Fenech, France
Class of 2019
- Avigayil Rapp, Boston, MA
Class of 2018
- Jason Jaramillo, Maimonides Medical Center, NY
Class of 2017
- Diana Sholomon, Brooklyn, NY
Class of 2022:
- Kristal Pouching, Mt. Sinai Medical Center, New York, NY
Class of 2021
- Shiran Porat, NYP Weill Cornell Medical Center, NY
Class of 2020
- Pratibha Sharma, Oregon Health Sciences University, OR
Class of 2023:
- Pin-Jung Chen, Cedars Sinai Medical Center, Los Angeles, CA
Class of 2022
- Brian Wolf, Maimonides Medical Center, NY
Class of 2021
- Kevin Shieh, University of California at Irvine, CA
Class of 2020
- Anna Urazov, Maimonides Medical Center, NY
- Jonathan Weltz, NYU Winthrop University, NY
- Natalie Elkayam, Maimonides Medical Center, NY
- Rajat Thawani, Oregon Health Sciences University, OR
Class of 2018
- Sudhamshi Toom, Maimonides Medical Center, NY
- David Chitty, Northwell Health, NY(Translational Research Fellowship)
Class of 2017
- Tsering Lama Tamang, University of California at Irvine, CA
Class of 2023
- Rabiah Ashraf, Essentia Health, Fargo, ND
- Sadia Aslam, Avera McKennan Univ Hospital, Sioux Falls, SD
- Jay Keith, PeaceHealth Southwest Medical Center, Vancouver, WA
- Sanjay Maheshwari, Reading Hospital – Tower Health, Reading, PA
- Tania Miah, Montefiore Medical Center – Weiler Center, Bronx, NY
- Bala Pushparaji, Cleveland Clinic, Cleveland, OH
- Syed Mazhar Uddin, Poplar Bluff Regional Med Center, St. Louis, MO
- Aarti Maharaj, University of Florida, Shands Hospital, Jacksonville, FL
- Htin Kyaw, Montefiore Medical Center – Weiler Center, Bronx, NY
- Arafat Farooqui, Washington University School of Medicine, St. Louis, MO
- Uyioghosa Asemota, Paris Regional Medical Center, Paris, TX
Class of 2022
- Gurchetan Randhawa, NYU, Manhattan
- Maham Waheed, Maimonides Medical Center, Brooklyn, NY
Class of 2021
- Awais Aslam, Essentia Health, ND
- Wei Jun Gu, Long Island Jewish Hospital, NY
- Aalia Mohamed Ghouse, Redington Fairview, ME
- Swetha Musty, Ascension Borgess Hospital, MI
- Ogochukwu Okoli, University of Maryland, MD
- Deborah Osafehinti, Spartanburg Regional M.C., SC
- Mohammad Saad Saeeduddin, Apogee Physicians, PA
- Karen Tuneev, Premier Health, OH
- Moaz Zia, Avera McKennan Hospital, SD
Class of 2020
- Behtash Saeidi, University of Toronto, Canada
- Celestine Mkpozi, Essentia Health, ND
- Neehal Wali, HSHS St. John’s Hospital, IL
- Sarwat Nasreen, Maimonides Medical Center, NY
- Maryam Baqir, Montefiore Wakefield, NY
- Vrunda Kelkar, CHI Franciscan Health System, WA
- Shaurya Sharma, Maimonides Medical Center, NY*
- Susan Lin, Maimonides Medical Center, NY
Class of 2019
- Eliza Sharma, St. Joseph’s Hospital, ME
- Nikhil Cordeiro, Mount Sinai Medical Center, NY
- Jacqueline Golden, Henry Ford Allegiance Health, MI
- Sruthi Namana, Porter Regional Hospital, IN
- Obinna Ibe, Charlotte Hungerford Hospital, CT
- Prameeta Jha, Decatur Memorial Hospital, IL
- Muhammad Sohail Yousuf, HSHS St. John’s Hospital, IL
- Husnain Waseem, Maimonides Medical Center, Brooklyn, NY
- Mariya Astashkevich, Maimonides Medical Center, Brooklyn, NY
- Shanti Patel, Yale New Haven Hospital, CT
- Abimbola Iluyomade, TX
Class of 2018
- Nijas Nazar, Montefiore Medical Center, NY
- Sabina Ratner, Stonybrook University, NY
- Sharonlin Bhardwaj, NYU Lutheran, NY
- Brian Poon, Good Samaritan Hospital, IL
- Oluwaseun Samuel, Vidant Medical Center, NC
Class of 2017
- Craig Feibusch, Summit Medical Group, NJ*
- Samson Alliu, Wright State University, OH** (Cardiology, Maimonides Medical Center, NY)
- Christos Christolias, NYP Lower Manhattan, NY
- Qing Luo
- Ramon Ortiz Espinal, Florida Flagler Hospital, FL
- Nishanth Pundru, Rhode Island Hospital, RI
- Hitesh Raheja, Cleveland Clinic, OH ** (Cardiology, Maimonides Medical Center, NY)
- Mark Gobrial, Henry Mayo Hospital, CA
- Neerva Rana, Henry Mayo Hospital, CA
- Radhika Voleti, Bayhealth Kent General Hospital, DE
- Betsy Kuriakose, Havasu Regional Medical Center, AZ
- Tanuj Sood, Washington Hospital Center, DC
- Vivek Kumar, Brigham and Women’s Hospital, MA
- Remigiusz Soltys, Trinitas Regional Medical Center, NJ
Class of 2023
- Amit Dhaliwal, (ID-Crit) NYU Langone Hospital, Long Island, Mineola, NY
Class of 2022
- Gurchetan Randhawa, NYU, Brooklyn, NY
- Laura Rivera-Boadla, Mount Sinai West, NY
Class of 2020
- Anuoluwapo Shobayo, Brown University, RI
Class of 2019
- Maria Jose Suarez Bohorquez, Maimonides Medical Center, Brooklyn, NY
Class of 2018
- Chiemeziem Nwanyanwu, Maimonides Medical Center, NY
- Jonathan Garellek, Northwell Health, NY
- Renata Kuperman, Maimonides Medical Center, NY*
Class of 2021
- Nyein Chann Wai Lynn, Washington University, St. Louis, MI
Class of 2020
- Joseph Gotesman, Northwell Lenox Hill Hospital, NY
Class of 2019
- Sanjana Kapoor, University of Pittsburgh, PA
Class of 2021
- Moshe Miller, University of Alabama, AL
- Orel Shuker, NYP Columbia and Cornell, NY
Class of 2017
- Amrita Sabharwal, University of California at Irvine, CA
Class of 2023:
- Brent Boodhai, University of Florida, Jacksonville, FL
- Kevin Clements, Maimonides Medical Center, Brooklyn, NY
- Thai Donenfeld, Maimonides Medical Center, Brooklyn, NY
Class of 2022
- Christiana Atuaka, Maimonides Medical Center, Brooklyn, NY
- Claudia De Arujo Duarte, Maimonides Medical Center, Brooklyn, NY
- Varun Tej Gonguntla, Elmhurst, Queens, NY*
- Carly Munro, Medstar Washington Hospital Center, Washington, DC
Class of 2021
- Angelica Fernandes, Rutgers New Jersey Medical School, Newark, NJ
- Sharad Oli, Wayne State University, MI
Class of 2020
- Aryeh Bernstein, Maimonides Medical Center, NY
- Carolyn Bendor-Grynbaum, University of Miami, FL
- Samuel Francis, Maimonides Medical Center, NY
Class of 2019
- Anna Abbasi, University of Missouri, MI*
- Ravi Karan Patti, Maimonides Medical Center, Brooklyn, NY
- Chetana Pendkar, SUNY Downstate, NY
- Arjun Saradna, University of Buffalo, NY
Class of 2018
- Precious Macauley, Westchester Medical Center, NY
- Ankur Sinha, Maimonides Medical Center, NY
- Parita Soni, Maimonides Medical Center, NY
Class of 2017
- Anisha Kamath, Winthrop University, NY
- Sushikumar Gupta, Maimonides Medical Center, Brooklyn, NY
- Omar Taha, Maimonides Medical Center, Brooklyn, NY
Class of 2022
- Kavish Singh, Dartmouth University, NH
Class of 2021
- Iqra Aftab, SUNY Downstate Brooklyn, NY
Class of 2020
- Krishna Kommineni, University of Tennessee, TN
Class of 2018
- Madina Abduraimova, SUNY Downstate, NY
- Sima Terebelo, SUNY Downstate, NY
Class of 2021
- Tayyaba Saeed, Anesthesiology, Maimonides Medical Center, Brooklyn, NY
- Ori Waksman, Cardiology Metabolism/Lipids, Mount Sinai, NY
Class of 2020
- Fidelis Okoli, NYU Medical Center, NY (Transplant Hepatology)
Class of 2019
- Jonathan Panitch, Hepatology, Montefiore Medical Center, NY
- Amy Espinal, Neurology, University of Chicago, IL
Class of 2018
- Alexa Sasson, University of Toronto, Canada (GI Research)
- Mahin Alamgir, Dermatology Residency, Rutgers RWJ, NJ
Class of 2017
- Shiv Raj, Cardiac Critical Care, Brigham and Women’s Hospital, MA** (Cardiology, Maimonides Medical Center, NY)
- Sabah Siddiqui, Cardiology Hypertension, VAMC Bronx, NY** (Cardiology, Maimonides Medical Center, NY)
- Bridget Gallagher, Hepatology, SUNY Downstate, NY
- Vasavi Devireddy, Physician Administration Fellowship Northwell, NY
Residency Overview
The Internal Medicine Residency Program at Maimonides Medical Center provides a unique educational experience, combining the outstanding clinical exposure of a major urban hospital with an emphasis on academic medicine. Our location, in the heart of Brooklyn, New York at the intersection of Borough Park and Sunset Park, and our designation as a safety net hospital, draw one of the most diverse patient populations in the US. Through exposure to both inpatient and outpatient medicine on the medical floors, the critical care and coronary care units, and the outpatient clinics, our residents become well-versed in all aspects of internal medicine, fully prepared to enter any practice setting or fellowship upon graduation.
The Program is fully accredited by the Accreditation Council of Graduate Medical Education (ACGME). We offer a total of 107 positions in two approved training programs:
- Categorical three-year residency, leading to eligibility for certification by the American Board of Internal Medicine (30 positions per year)
- Preliminary one-year internal medicine program for those pursuing specialty training in other areas (up to 5 a year)
The Department of Medicine has divisions in the following specialties:
- Critical Care Medicine
- Endocrinology and Metabolism
- Gastroenterology
- Hospital-based Internal Medicine
- Geriatrics
- Hematology/Oncology
- Infectious Diseases
- Nephrology
- Primary Care Internal Medicine
- Pulmonary Medicine
- Rheumatology and Immunology
- Supportive Care (Palliative Medicine)
Maimonides offers in-house fellowships in the following medical subspecialties:
- Cardiovascular Medicine and Interventional Cardiology
- Critical Care Medicine
- Gastroenterology
- Geriatrics
- Hematology/Oncology
- Infectious Diseases
- Nephrology
- Pulmonary Diseases
Program Leadership

Residency Program Director of the Department of Internal Medicine at Maimonides Medical Center
Assistant Professor of Medicine at SUNY Downstate Medical Center
Hometown: Sangrur, Punjab in India
Medical School: Government Medical College, Amritsar, Punjab, India.
Residency: Maimonides Medical Center, Brooklyn, NY
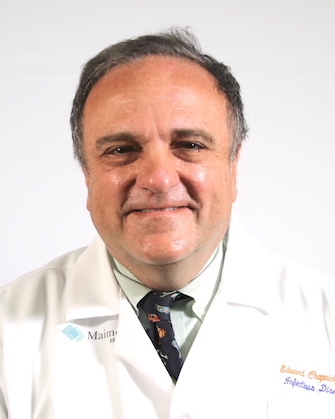
Chair of Medicine at Maimonides Medical Center
Director, Infectious Diseases Division
Professor of Clinical Medicine at SUNY Downstate College of Medicine
Hometown: Flushing, N.Y.
Medical School: SUNY Downstate
Residency, Fellowship: Maimonides Medical Center
Associate Program Directors
Hometown: Roslyn, New York
Medical School: St. George’s University School of Medicine
Residency: New York-Presbyterian Brooklyn Methodist Hospital

Hometown: Delhi, India
Medical School: Himalayan Institute of Medical Sciences, Baksar Wala, India
Residency: SUNY Downstate Medical School
Fellowship: Endocrinology at SUNY Downstate Medical School

Hometown: Staten Island, NY
Medical School: Ross University School of Medicine
Residency: NYU Langone Health
Fellowship: Geriatrics at Mt. Sinai Hospital

Hometown: Dumont, New York
Medical School: NYU School of Medicine
Residency: Bellevue Hospital – NYU School of Medicine

Hometown: Moscow, Russia
Medical School: Russian State Medical Pirogov University in Moscow, Russia
Residency: Maimonides Medical Center
Hometown: Amritsar, Punjab
Medical School: Dr. D.Y. Patil Medical College, Kolhapur, Maharashtra
Residency: Maimonides Medical Center
Fellowship: Pulmonary and Critical Care at Maimonides Medical Center

Hometown: Yangon, Myanmar
Medical School: University of Medicine 1, Yangon
Residency: Long Island College Hospital
Fellowship: Infectious Disease at Maimonides Medical Center
Residency Curriculum
The internal medicine curriculum at Maimonides fulfills the requirements of the Residency Review Committee for Internal Medicine (RCC-IM) of the Accreditation Council for Graduate Medical Education (ACGME). The Categorical Internal Medicine Residency Program is a three-year ACGME accredited program based around a 4+1 block system comprising 4 weeks of inpatient and subspecialty elective rotations alternating with 1 week of primary care ambulatory medicine. Our comprehensive curriculum is focused on engaging residents as adult learners with the aim of producing competent, curious and compassionate internists. The curriculum offers broad and balanced experience in both inpatient and outpatient settings, which prepare the graduate for a career in general internal medicine or further training in any of the medical subspecialties.
By the end of the three-year program, graduating residents leave as expert practitioners in the care and treatment of major acute and chronic diseases.
Preliminary Medicine
Our one-year Preliminary Medicine Program provides interns with a comprehensive exposure to internal medicine, providing them with a strong foundation for their future advanced training. Preliminary interns work side-by-side with their Categorical intern colleagues, managing patients both on the medical floors and the intensive care unit. These experiences are interspersed throughout the year with a generous number of elective weeks, allowing the Preliminary intern to customize their educational program to what will best suit their future endeavors. Our Preliminary interns emerge from their year at Maimonides adept in the management of patients with a wide range of complex internal medicine diagnoses, ready to take on their advanced program training.
The Residency Program incorporates training in many areas, including:
- Preventive medicine
- High quality, cost-effective patient care
- Cultural diversity
- Communication skills
- Biomedical ethics
Comprehensive Inpatient and Outpatient Experiences
We offer a 4+1 schedule, which separates inpatient and outpatient experiences, enhancing the education in both settings.
Inpatient rotations include the general medical floors, medical and coronary care units (ICU/CCU) and specialty divisions. Under the supervision of the full-time faculty, residents participate in daily rounds on each unit. Responsibilities include:
- Completing patient evaluations
- Developing treatment plans
- Performing procedures
- Writing patient orders
- Responsibility for the ongoing care and monitoring of patients in the 20-bed medical intensive care unit and the 10-bed cardiac intensive care unit
- Working with an interdisciplinary team including social services, case management, nursing, wound care, and nutritional support staff
Our Medicine wards are comprised of four large geographically based general medicine teams, each supervised by three attending physicians. This system ensures that our trainees receive an excellent educational experience while providing the highest level of patient safety and care. We also have a night medicine rotation under the supervision of in-house faculty physicians. There, the overnight residents and interns practice the art of the initial assessment and management of newly presenting patients while helping with the ongoing care of established patients.
The inpatient rotation is enriched by the following academic activities:
- A weekly Intern Report allows PGY1s to learn the basic principles of patient management, proper history and physical examination skills, as well as honing their presentation and diagnostic skills.
- Morning and Noon Report focuses on case presentations. Led by the Chief Residents and guided by Program leadership and faculty physicians, this is an opportunity for residents to learn about differential diagnosis building and evidence-based patient management in a safe and structured environment.
- ABIM preparation is done during weekly Board Review sessions in the morning, where senior residents analyze information on the format and content of the certification exam, with the guidance of the Program leadership. Additionally, a 5-month Board Preparation course driven by subspecialists is conducted in the latter half of PGY-3 year to aid candidates prepare for their exam.
- Journal Club is a resident-driven discussion about published articles, supported by Program leadership and faculty physicians. This educational meeting provides a forum for a collective effort to keep up with the current literature.
- The program leadership, faculty physicians and guest speakers lead bi-monthly Grand Round presentations, providing residents a valuable discussion that can affect patient’s treatment and care planning.
- Monthly M&M lectures foster a climate of openness and discussion about medical errors while providing an interdisciplinary forum to teach curriculum on quality improvement and medico legal issues.
The outpatient curriculum offers ambulatory care experiences in the primary care clinic, private office practice settings, and specialty clinics. Categorical Medicine residents spend a week every fifth week at their longitudinal continuity clinic, assigned to one of three primary care sites. Residents act as primary providers for a panel of patients, with oversight by our outpatient faculty.
Additionally, the outpatient week has structured protected time, including:
- Wednesday Academic Day, consists on a one-hour morning report, a two-hour research support session, and an hour with our director of the mindfulness program where he trains residents in humanism and awareness techniques, followed by Journal Club. The remainder of the Academic Day is spent immersed in experiential learning in our state-of-the-art simulation lab, which boasts a virtual reality simulator, interactive ultrasound simulation and practice performing procedures on mannequins.
- Friday morning case-based primary care didactics, a resident-led teaching session that allows participants to gain experience in teaching each other evidence-based, high yield primary care topics.
- Friday Resident Wellness Half-Day, used by residents to catch up on academic work and/or self-care.
All of the above experiences provide residents with an understanding of the full range of care and support services available to patients. Our program prepares residents for the complexities of healthcare delivery in today’s world, while attending to their well-being.
The Humanism Project
The Humanism Project focuses on developing communication skills, recognizing unconscious bias, and understanding medical ethics. This innovative project helps residents navigate the unique but interdependent needs of patients, colleagues, families, and themselves, by developing self-awareness and a sensitivity to interpersonal dynamics and complex topics that are not always addressed by a formal curriculum. Its goal is to develop physicians who are patient-centric, professional, empathetic, and emotionally fulfilled in their medical careers. These sessions combine standardized patient scenarios, small group discussions, experiential learning, reflection sessions, and trips to the community.
Our Research Department
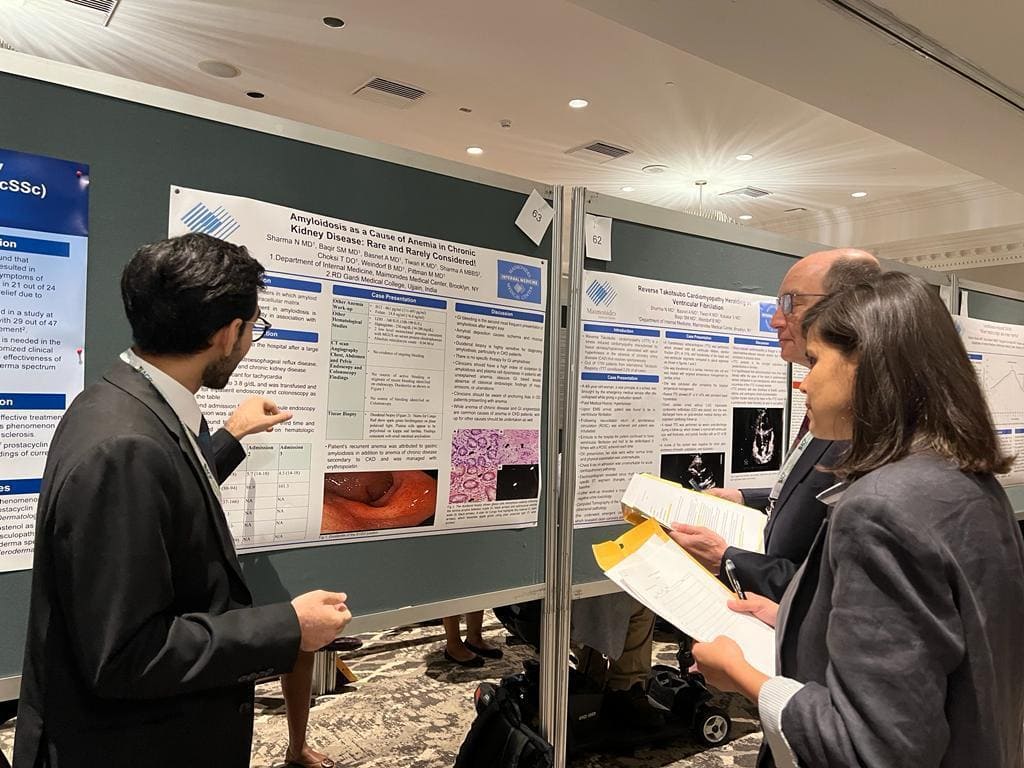
All residents in the Department of Medicine at Maimonides are required to pursue scholarly endeavors, including quality improvement and clinical research. We have dedicated research associates, divisional research liaisons and statisticians available to guide residents through study design, IRB approval and research funding.
Our Director of Resident Research, Dr. Yu Shia Lin, and our Chief Residents personally help residents to identify and select appropriate research topics aligned with their career plans and specialty interests. The research leadership is also available to mentor and review residents’ research projects, abstracts and manuscripts prior to conference presentations and journal submission for publication. We also have an in-house biostatistician available for consultation on any project at any stage of development, as well as to assist with data analysis.
The department has an academic curriculum and faculty members dedicated to help residents conduct quality improvement and patient safety projects. Residents and attending physicians are also encouraged to take an active role in our monthly quality improvement meetings, where patient quality and safety issues are discussed among an interdisciplinary team. Additionally, Maimonides organizes an interdepartmental Resident Quality Council, which enables residents to take an active role in the hospital-wide quality initiatives.
Maimonides strongly supports resident’s research endeavors. Our residents present at many national and regional scientific meetings, having won national awards for both clinical and basic science research over the last several years.
Department of Medicine, Research Administration
Dr. Edward Chapnick | Chair of Medicine
Dr. Navjot Somal | Program Director
Dr. Yu Shia Lin | Director of Research
Dr. Alana Zanetti-Yabur | Chief Resident, Research
Dr. Tejaswi Venigalla | Chief Resident, Research
Aditi Parulkar | Research Volunteer
Asiya Batool | Research Volunteer
Aye Honey Aung | Research Volunteer
Cherry Maung Maung Aye | Research Volunteer
Hashim Khan | Research Volunteer
Kantash Kumar | Research Volunteer
Khin Htet Htet Soe | Research Volunteer
Khin Wathan | Research Volunteer
Laiz Darwich | Research Volunteer
Maha Tariq | Research Volunteer
May Thet Hmu Tun | Research Volunteer
May Zin | Research Volunteer
Patrick DeSanto | Research Volunteer
Tin Mee Mee Aung | Research Volunteer
Divisional Research Liaisons
Dr. Benjamin Weindorf | General Internal Medicine
Dr. Ira Mayer | Gastroenterology
Dr. Jennifer Breznay | Geriatrics
Dr. Yiqing Xu | Hematology/Oncology
Dr. Yu Shia Lin | Infectious Diseases
Dr. Jocelyne Karam | Metabolism & Endocrinology
Dr. Sheldon Greenberg | Nephrology
Dr. Chernyak | Neurology
Dr. Egan | Palliative Care
Dr. William Pascal | Pulmonary & Critical Care
Dr. Schiff | Rheumatology & Immunology
- Khan O, Raashid S, Hashim M, Clements K, Maheshwari S, Uddin SM, Siriya P, Vadsariya A, Park P, Pascal W. Diagnosis of adrenocortical carcinoma with hypercortisolism in a patient presenting with hypokalemic metabolic alkalosis. Journal of Community Hospital Internal Medicine Perspectives. 2022;12(5):114-8.
- Achuthanandan S, Dhaliwal A, Lu T, Sharma K. Brain Abscess Due to Lactobacillus Fermentum in an Uncontrolled Diabetic. Cureus. 2022 Jun 27;14(6).
- Mubashir T, Balogh J, Breland E, Rumpel D, Waheed MA, Lai H, Napolitano CA. Risk Factors and Outcomes of Protein-Calorie Malnutrition in Chronic Heart Failure Patients Undergoing Elective Cardiac Surgery. Cureus. 2022 Oct 17;14(10).
- Pulverenti TS, Zaaya M, Knikou M. Brain and spinal cord paired stimulation coupled with locomotor training affects polysynaptic flexion reflex circuits in human spinal cord injury. Experimental Brain Research. 2022 Jun;240(6):1687-99.
- Lue AM, Richards-Dawson MA, Gordon-Strachan GM, Kodilinye SM, Dunkley-Thompson JA, James-Powell TD, Pryce CA, Mears CD, Anzinger JJ, Webster-Kerr K, Christie CD. Severity and Outcomes of Dengue in Hospitalized Jamaican Children in 2018–2019 During an Epidemic Surge in the Americas. Frontiers in Medicine. 2022;9.
- Donenfeld T, Basnet A, Harris C, Waheed M. Accessibility and Content of Fellowship Programs for Cardiovascular Disease. Cureus. 2022 Jun 15;14(6).
- Olawoye A, Kyaw H, Nwosu IF, Ibeson CE, Miah T, Weindorf B, Donenfeld T, Basnet A, Adaramola O, Nsofor GC, Adebayo AA. Isolated Superior Mesenteric Artery Dissection: An Unusual Etiology of Epigastric Pain. Cureus. 2022 Jun 6;14(6).
- Sharma N, Zivari K, Kaur A, Kureshi A, Mayer I. Fish Bone-Induced Pancreatitis. Cureus. 2022 Jun 22;14(6).
- Perice L, Naraghi L, Likourezos A, Singh H, Haines L. Implementation of a novel digital ultrasound education tool into an emergency medicine rotation: UltrasoundBox. AEM Education and Training. 2022 Jun;6(3):e10765.
- Uzzan M, Martin JC, Mesin L, Livanos AE, Castro-Dopico T, Huang R, Petralia F, Magri G, Kumar S, Zhao Q, Rosenstein AK, Singh H. Ulcerative colitis is characterized by a plasmablast-skewed humoral response associated with disease activity. Nature medicine. 2022 Apr;28(4):766-79
- Maharaj A, Boodhai B, Somal N, Brejt S. Non-ST elevation myocardial infarction as the initial presentation of chronic eosinophilic leukemia: A case report.
- Maharaj A, Jana K, Boodhai B, Janga KC, Fein E, Greenberg S. Central diabetes insipidus after total abdominal hysterectomy and bilateral salpingo‐oophrectomy: A case report. Clinical Case Reports. 2022 Mar;10(3):e05481
- Somal N, Karan R, Maharaj A, Halperin J, Boodhai B, Lipton J, Masri DJ, Kumar K. Dysphagia, an uncommon initial presentation of sarcoidosis. Respiratory Medicine Case Reports. 2022 Jan 1;37:101647.
- Boodhai B, Maharaj A, Rodriguez CA, Lin YS. Re-exposure causing rapid onset of vancomycin induced thrombocytopenia. IDCases. 2022 Jan 1;27:e01398.
- Kyaw H, Shajahan S, Gulati A, Synn S, Khurana S, Nazar N, Shrestha S, Kerstein J. COVID-19 mRNA Vaccine-Associated Myocarditis. Cureus. 2022 Jan 7;14(1).
- Kumari N, Sharma N, Krishnan V. Beetle wing inspired fabrication of nanojunction based biomimetic SERS substrates for sensitive detection of analytes. Materials Technology. 2022 Jan 28;37(2):112-23.
- Sharma N, Zivari K, Yunina D, Grunwald M, Azar O, Rahmani R, Tin K. Strongyloides stercoralis Infection in Immunocompromised Host. Cureus. 2022 Jan 13;14(1).
- Kaur A, Zivari K, Sharma N. What Happens When the Digested Screw Does Not Come Out of Ileum? Cureus. 2021 Dec 4;13(12).
- Shah H, Bari M, Kaur J, Al Janabi N, Kaur M, Soneghet R, Patel N, Patel A, Siddiqui F. Trends and Factors Associated with Utilization of Palliative Care among Hospitalizations Due to End Stage COPD. Chest. 2021 Oct 1;160(4):A1936.
- Shah H, Kaur J, Kaur M, Al Janabi N, Soneghet R, Bari M, Patel K, Upadhyaya A, Siddiqui F. Outcomes of Palliative Care Hospitalizations due to End Stage COPD. Chest. 2021 Oct 1;160(4):A1939.
- Raheja H, Waheed M, Harris C, Patel N, Hashmi A, Kundal S, Patel J, Malik B, Frankel R, Shani J. Racial disparities in the use of mechanical circulatory support devices in cardiogenic shock. European Heart Journal. 2021 Oct;42(Supplement_1):ehab724-1484.
- Zivari K, Sharma N, Kaur A, Kureshi A, Yakubov S, Mayer IE. S1474 Fishbone-Induced Pancreatitis. Official journal of the American College of Gastroenterology| ACG. 2021 Oct 1;116:S674-5.
- Sharma N, Zivari K, Kaur A, Pittman ME, Niknam N. S1732 ORISE-Gel Masquerading as a Colonic Polyp. Official journal of the American College of Gastroenterology| ACG. 2021 Oct 1;116:S769.
- Kaur A, Zivari K, Sharma N, Patel K, Rahmani R, Iswara K. S3047 Small Intestinal Adenocarcinoma: Rarely Considered, Often Missed on Endoscopy. Official journal of the American College of Gastroenterology| ACG. 2021 Oct 1;116:S1258-9.
- Sharma N, Zivari K, Kaur A, Pittman ME, Rahmani R, Tin K. S1508 Challenges of Treating Type 2 Autoimmune Pancreatitis Mimicking Pancreatic Cancer. Official journal of the American College of Gastroenterology| ACG. 2021 Oct 1;116:S688.
- Kaur A, Zivari K, Sharma N, Zafar F, Grunwald MD, Iswara K. S1885 Removing a Foreign Body from Ileum: What Happens When the Screw Does Not Come Out. Official journal of the American College of Gastroenterology| ACG. 2021 Oct 1;116:S828.
- Zaaya M, Pulverenti TS, Knikou M. Transspinal stimulation and step training alter function of spinal networks in complete spinal cord injury. Spinal Cord Series and Cases. 2021 Jul 3;7(1):1-8.
- Swaminathan G, Nguyen LP, Namkoong H, Pan J, Haileselassie Y, Patel A, Ji AR, Mikhail DM, Dinh TT, Singh H, Liao B. The aryl hydrocarbon receptor regulates expression of mucosal trafficking receptor GPR15. Mucosal immunology. 2021 Jul;14(4):852-61.
- Pulverenti TS, Zaaya M, Grabowski M, Grabowski E, Islam MA, Li J, Murray LM, Knikou M. Neurophysiological changes after paired brain and spinal cord stimulation coupled with locomotor training in human spinal cord injury. Frontiers in Neurology. 2021 May 10;12:627975.
- Randhawa J, Kaur J, Randhawa HS, Kaur S, Singh H. Thrombosis of the portal vein and superior mesenteric vein in a patient with subclinical COVID-19 infection. Cureus. 2021 Apr 8;13(4).
- Raheja H, Chukwuka N, Agarwal C, Sharma D, Munoz-Martinez A, Fogel J, Khalid M, Hashmi AT, Ehrlich S, Waheed MA, Siddiqui S. Should COVID-19 patients> 75 years be ventilated? An outcome study. QJM: An International Journal of Medicine. 2021 Mar;114(3):182-9.
- Waheed MA, Khalid M, Hashmi AT, Shani J, Malik B. Recurrent Takotsubo Cardiomyopathy Presenting With Anterior Wall ST-Elevation Myocardial Infarction. Cureus. 2021 Feb 20;13(2).
- Gonuguntla VT, Wolf L, Chen P-J, Miah T, Margulis Y, (2021) Case report, Acute inflammatory demyelinating polyneuropathy as the first manifestation of systemic lupus erythematosus
- Rojas-Marte G, Hashmi AT, Khalid M, Chukwuka N, Fogel J, Munoz-Martinez A, Ehrlich S, Waheed MA, Sharma D, Sharma S, Aslam A. Outcomes in patients with COVID-19 disease and high oxygen requirements. Journal of clinical medicine research. 2021 Jan;13(1):26.
- Waheed MA, Rojas-Marte G. Recurrent Acute Pericarditis Triggered by COVID-19 Disease. Cardiology and Cardiovascular Medicine. 2021;5(2):218-23.
- Naeem A, Malik AA, Rana RA, Hassan G, Afzal F. Hemostatic Spray; A Rescue to Severe Post-pancreaticoduodenectomy Hemorrhage-A Novel Technique to use. Journal of Surgery and Research. 2021;4:616-20.
- Seecheran N, Boodhai B, Maharaj A, Ramdeen A, Debideen N, Ochalal V, Singh R, Seecheran R, Seecheran V, Persad S, Abdullah H. The effect of low-dose ticagrelor on platelet function profiles in patients with stable coronary artery disease in Trinidad: the TWIST pilot study. Cardiology and Therapy. 2020 Dec;9(2):493-503.
- Sharma S, Kommineni K, Mehta SS, Singh H. Lorlatinib-associated acute respiratory distress syndrome. American Journal of Therapeutics. 2020 Nov 1;27(6):e698-9.
- Waheed MA, Khalid M, Hashmi AT, Malyshev Y, Ayzenberg S. Acute Pulmonary Embolism Presenting With Angina and a Positive Cardiac Stress Test. Cureus. 2020 Oct 17;12(10).
- Rojas-Marte G, Khalid M, Mukhtar O, Hashmi AT, Waheed MA, Ehrlich S, Aslam A, Siddiqui S, Agarwal C, Malyshev Y, Henriquez-Felipe C. Outcomes in patients with severe COVID-19 disease treated with tocilizumab: a case–controlled study. QJM: An International Journal of Medicine. 2020 Aug 1;113(8):546-50.
- Islam MA, Zaaya M, Comiskey E, Demetrio J, O’Keefe A, Palazzo N, Pulverenti TS, Knikou M. Modulation of soleus H-reflex excitability following cervical transspinal conditioning stimulation in humans. Neuroscience Letters. 2020 Jul 27;732:135052.
- Sharma N, Landsberg E, Kumar V, Gambhir HS. A Curious Case of Hypervitaminosis D. Cureus. 2020 Jun 8;12(6).
- Zaaya M, Pulverenti TS, Islam MA, Knikou M. Transspinal stimulation downregulates activity of flexor locomotor networks during walking in humans. Journal of Electromyography and Kinesiology. 2020 Jun 1;52:102420.
- Munoz-Martinez A, Waheed MA, Jhaveri KD, Rojas-Marte G. COVID-19 related rhabdomyolysis.
- Elliot S, Periera-Simon S, Xia X, Catanuto P, Rubio G, Shahzeidi S, El Salem F, Shapiro J, Briegel K, Korach KS, Glassberg MK. MicroRNA let-7 downregulates ligand-independent estrogen receptor–mediated male-predominant pulmonary fibrosis. American journal of respiratory and critical care medicine. 2019 Nov 15;200(10):1246-57.
- Sharma N, Darr U, Darr A, Sood G. Stauffer syndrome: a comprehensive review of the icteric variant of the syndrome. Cureus. 2019 Oct 30;11(10).
- Seecheran N, Seebalack V, Seecheran R, Maharaj A, Boodhai B, Seecheran V, Persad S, Motilal S, Tello-Montoliu A, Schneider D. TRimetazidine as an Agent to affeCt clopidogrEl Response: the TRACER study. Cardiology and Therapy. 2019 Dec;8(2):229-37.
- Naumeri F, Naeem A, Khalid MS, Sohail M. Variability of presentation and surgical approach in Congenital Cystic Lesions of Lung: A retrospective study in children presenting in Mayo Hospital. JPMA. 2019 Jul.
- Sharma N, Darr U, Darr A, Sood GK. Macro-aspartate aminotransferase: misleading finding in a patient with non-alcoholic fatty liver disease. Cureus. 2019 Jun 29;11(6).
- Seecheran NA, Maharaj A, Boodhai B, Seecheran R, Seecheran V, Persad S, Ramsaroop K, Sandy S, Giddings S, Sakhamuri S, Ali R. Prevalence of clOpidogrel ‘resIstaNce’in a selected population of patients undergoing elective percutaneous coronary intervention at a tertiary cardiovascular centre in Trinidad: the POINT pilot study. Open Heart. 2019 Feb 1;6(1):e000841.
- Naeem A, Khan U, Ali A. Effect of excessive mobile phone usage (Hours) on sleep patterns among the medical students of King Edward Medical University Lahore. Indo American Jouranl of pharmaceutical sciences. 2018 Jul 1;5(7):6400-5.
- Elliot S, Rubio G, Xia X, Catanuto P, Pereira-Simon S, Shapiro J, Glassberg MK, Pastar I, Tomic-Canic M, Glinos G. Therapeutic benefits of exosomes derived from mesenchymal stromal cells in bleomycin-induced pulmonary fibrosis in aged mice.
- Seecheran N, Nandlal N, Nankissoon S, Nancoo C, Nelson C, Nkemakolam A, Noel N, Olivers K, Parasram R, Rodriguez M, Seecheran R. A, Maharaj A. A Trinidadian cardiovascular medication adherence survey: the ADHERE TNT study. Int J Comm Med Public Health. 2017 Oct;4:3601.
- Clement YN, Mahase V, Jagroop A, Kissoon K, Maharaj A, Mathura P, Quan CM, Ramadhin D, Mohammed C. Herbal remedies and functional foods used by cancer patients attending specialty oncology clinics in Trinidad. BMC complementary and alternative medicine. 2016 Dec;16(1):1-7.
- Maharaj A, Cook J, Lalchan SA, Suite M, Barrow S, Lalchan MS. Sarcoid Tattoo Granuloma and Ocular Sarcoidosis: The Great Masquerader. Published online September 16, 2016
- Sharma S, Singh H. Glaucoma: Risk Factors and Prevalence: A Review. Int J Com Health and Med Res. 2016;2(2):66-72.
- Maharaj A, Singh VR, Lalchan SA. Lisch and the Importance of His Nodules. The West Indian Medical Journal. 2014 Dec;63(7):799.
- Hemat S, Takano T, Kizuki M, Mashal T. Health-care provision factors associated with child immunization coverage in a city centre and a rural area in Kabul, Afghanistan. Vaccine. 2009 May 11;27(21):2823-9.
Why Choose Maimonides?
At Maimonides, we provide a superb internal medical education. Our highly engaged faculty provide expert guidance to the residents in caring for an incredibly broad-based population here in the heart of the amazing borough of Brooklyn, New York. Over their three years of training, residents manage a rich and diverse array of patients with remarkably wide-ranging underlying pathologies.
Maimonides Medical Center
Founded in 1911, Maimonides has been a cornerstone of the Brooklyn community and is the largest hospital in Brooklyn. Over the last century, we have become a world-class care center and a vital part of New York City. Maimonides Medical Center is the top five largest independent teaching hospitals in the country.
From the first heart transplant in the U.S. to the first hospital-based Clinical Simulation Center in the Northeast, we are on the cutting edge of innovation. For several years, Maimonides has been rated among the ‘Top 10 Hospitals’ in the Nation for Clinical Excellence according to data published by the U.S. Centers for Medicare & Medicaid Services.
Maimonides Medical Center
- #1 in U.S. for heart attack survival
- #1 in New York State for outcomes from percutaneous coronary intervention
- An innovative program in Bloodless Medicine & Surgery
- Top 1% in the US for stroke patient outcomes
- Comprehensive Breast Center
- Nationally recognized Cancer Center
- Prostate Center with the most advanced HIFU technology
- State-of-the-art Bone and Joint Center
- Nationally recognized Neonatal Intensive Care Unit (NICU)
- Brooklyn’s only comprehensive Children’s Hospital
- Brooklyn’s first interdisciplinary Pelvic Floor Center
Our Location
Maimonides is unique because it is located within the heart of the bustling borough of Brooklyn, New York. This leads to an amazingly diverse patient population with a wide array of pathology. Maimonides offers a unique opportunity for training in a high-acuity and busy tertiary care center which also serves as a safety-net community hospital. Residents leave this program able to manage any medical challenge that comes their way.
New York City is one of the most vibrant and exciting cities in the world. While completing residency in New York, you will have access to theater, music, endless restaurants, sporting events, and much more. Whatever your interests, you will be able to find things to do throughout the boroughs of New York. Brooklyn itself is full of rich history and unique neighborhoods everywhere you look. It boasts quirky cafes, hip brunch spots, beautiful parks, excellent schools, and a strong sense of community.
Resident Stories
How To Apply
All applications are accepted only through the Electronic Residency Application Service (ERAS) and are then reviewed by our Selection Committee. The Department of Medicine offers all of its residency positions through the National Resident Matching Program (NRMP).
The review of your application and the scheduling of interviews requires a completed ERAS application, including the following components:
- Medical Student Performance Evaluation (MSPE – Dean’s Letter)
- Medical school transcript(s)
- USMLE/COMLEX transcripts
- Three (3) letters of recommendation (at least one of which should be from a department of medicine)
- Personal statement
- Curriculum Vitae
Maimonides Medical Center complies with federal and city laws and orders prohibiting discrimination in employment. Such discrimination includes race, creed, color, national origin, sex, age, handicap, marital status or sexual orientation.
Program Requirements
- We sponsor H1B and J1 visas if necessary. No visa type is guaranteed. For H1B Visas, we require proof of passing Step 3 by the NRMP Rank Order List due date to ensure that an H1B visa can be issued in time for a July 1 start date.
- We do not have strict minimum USMLE/COMLEX score requirements; however, we do consider both scores and number of attempts.
- For international graduates, we do not require U.S. clinical experience, but it is strongly favored.
- We prefer candidates who have graduated from medical school within the last three years, but we will consider more than three years from date of graduation with commensurate clinical experience in the intervening time.
- Applicants must designate their interest in either the Preliminary or the Categorical Internal Medicine Program, as we do not accept applications to both programs from the same candidate.
Interview Day
In adherence with national standards, all interview days will be held virtually this season. The interview session typically includes presentations from the Program Director and the Chief Residents as well as a greeting from the Chair of Medicine. Each candidate will interview with a faculty member and with a current resident, as well as with a Chief Resident or Associate Program Director. Applicants will also have allocated time to meet briefly with the Program Director. Finally, there will be an interactive group session with our current residents, so that candidates can learn more about our residents’ experiences at Maimonides.
© 2020 Maimonides Medical Center
